Lumbar osteochondrosis is a neurological disorder of the spine affecting people of all ages in which degenerative dystrophic changes occur in the lumbar spine. They affect intervertebral discs, articular cartilage, bone tissue.
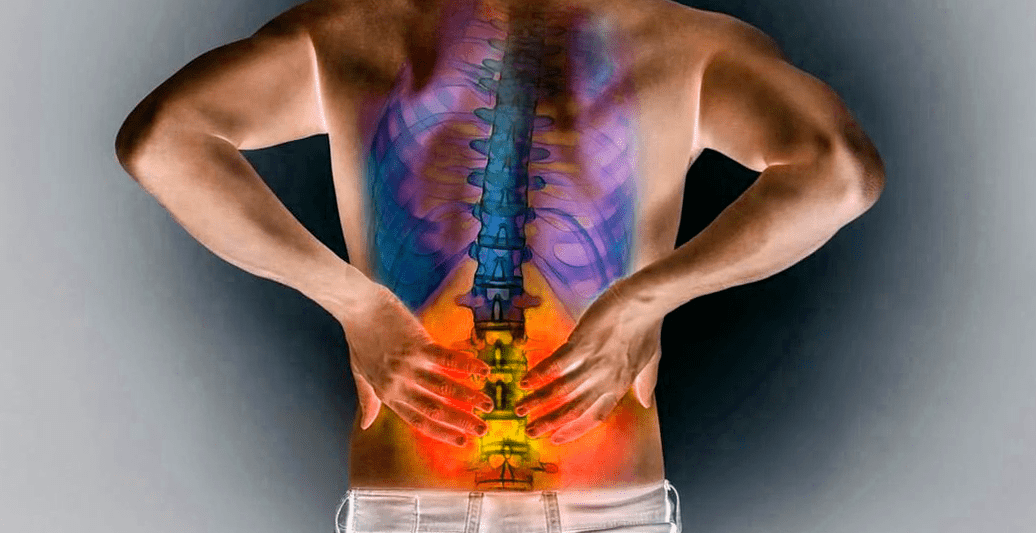
The cause of this disease is the severe stress the lower back experiences on a daily basis - when walking, sitting, lifting weights. It is important to start treatment of osteochondrosis as early as possible in order to avoid possible complications. Osteochondrosis of the lumbar spine is a fairly complex disease requiring complex treatment under the supervision of an experienced specialist.
Main features
Lumbosacral osteochondrosis is a degenerative dystrophic disease of the articular cartilage of the spine located in the lumbar spine. In other words, the disease means the destruction of the cartilaginous discs that lie between the vertebral bodies. The mobility of the vertebrae decreases, the distance between them decreases, and compression (compression) of the nerve endings occurs.
The lumbosacral spine is more susceptible than other spines because the greatest load falls on it. Doctors accurately diagnose osteochondrosis in 80 percent of patients who complain of back pain. The disease begins with the breakdown of glycoproteins in connective tissue, and it is these compounds that give it elasticity. The intervertebral disc is the first to suffer from this process.
Each intervertebral disc consists of a nucleus and an outer annulus. After the core dries, the disc loses its elasticity and the annulus ruptures and delaminates. Through the gap in the ring, the nucleus can fall off (form a hernia).
As a result of these processes, the load on the vertebrae increases significantly, and the body responds to this by a dramatic increase in the formation of bone tissue where the load increases.
which vertebrae are affected
The lumbar region consists of five vertebrae: L1-L5, with the fifth vertebra connected to the sacrum. The intervertebral discs between them are most often affected by osteochondrosis.
There are several types of lumbosacral osteochondrosis, which differ in the location of the vertebrae.
- Disorders of the upper lumbar spine (1, 2 and 3 vertebrae).
- Disorders at the level of the lower lumbar spine (3, 4 and 5 vertebrae).
- Sacral osteochondrosis (located in the sacrum). This type of disease is very rare.
- The bones of the sacrum and vertebrae are fused.
Developmental stages of lumbosacral osteochondrosis
There are four (sometimes three) stages of lumbosacral osteochondrosis. Here they come:
- The nuclei and their positions have changed.
- The outer annulus begins to break down.
- After the ring ruptures, the nucleus falls off.
- The destructive process affects vertebrae, joints, ligaments.
In the first stage of lumbosacral osteochondrosis, a person experiences some discomfort and pain in the lower back. It may be acute or painful in nature. Muscles and blood vessels spasm, problems with organ function.
Vasospasm of the lower extremities can lead to atherosclerosis and bladder dysfunction.
In the second stage, the back muscles are constantly tense due to the instability of the vertebrae. Patients complain of lower back fatigue, discomfort, and uncertainty.
In the third stage, the intervertebral disc nucleus detaches from the annulus fibrosus, forming an intervertebral hernia. Fallen disc fragments can trap nerve roots that innervate internal organs, muscles, and areas of the skin. As a result, the sensitivity of an area changes, and there may be burning, numbness, and loss of sensitivity. Compressed nerves can lead to loss of motor function or muscle wasting.
Based on the area of damaged innervation, doctors can tell exactly where the spinal cord is damaged. If fragments of the disc fall into the spinal canal, the spinal cord is pinched. This often disrupts the function of the pelvic organs and the motor function of the lower extremities.
In the fourth stage, the disc tissue is completely replaced with dense connective tissue. The support function of the spine is restored, and the pain is relieved, but the mobility and elasticity are lost.
The above-mentioned stages are conditional because the development of the disease is very individual.
Symptoms: Your Body Will Tell You
Symptoms can be divided into primary symptoms related to spinal changes and additional symptoms related to impaired innervation due to nerve compression.
Main:
- Lower back pain and numbness. At first, it may be temporary and manifest with physical exertion and exercise. As they develop, they become permanent and can be sharp or painful, even when coughing or sneezing;
- fatigue and depression;
- Decreased lower extremity sensitivity;
- Impaired lower back mobility;
- Curvature of the spine, lordosis.
additional:
- severe back pain;
- deterioration of reflexes;
- lower extremity shooting, lameness;
- muscle weakness;
- decreased sweating;
- Feeling of cold legs.
Pain is observed in different parts of the body depending on the localization of the osteochondrosis:
- Damage to 1-2 vertebrae - in the groin area;
- Damage to 3-4 vertebrae - calf and thigh area;
- With the failure of the fifth vertebra - in the sacrum, lower back.
How is lumbosacral osteochondrosis diagnosed?
Diagnosis begins with a detailed investigation of the patient. Physicians should listen carefully to patients' complaints to identify the location and intensity of pain, paying particular attention to side effects (loss of skin sensitivity, impaired motor function).
Physicians must track the development of symptoms over time, analyzing the nature and effectiveness of previous treatment (or self-treatment). In addition, physicians should pay attention to the medical history and ask about the patient's lifestyle, work situation, and previous medical conditions.
Special attention should be paid to posture, as the spine may be curved. It is worth noting how the patient moves and how well the muscles develop.
The main diagnostic tool for lumbosacral osteochondrosis is radiography. MRI and computed tomography have been used successfully.
reason
The lumbosacral region has many unique features. The spinal cord terminates at the level of the 12th thoracic-1 lumbar vertebrae. In the lumbosacral region there are spinal nerve fibers, which gather into bundles. The lumbar spine and sacral roots form the sciatic nerve.
The main feature of this part of the spine is the large loads (dynamic and static) that he constantly experiences. This is why the lumbar discs wear out earlier.
possible consequences
The consequences of this disease are dangerous:
- Damage to the knee and pelvic joints;
- Visceral organ dysfunction (problems with the potency of male and female reproductive organs);
- low back pain, sciatica and low back pain;
- Compression of the spinal cord, resulting in impaired reflexes;
- Inflammation of the sciatic nerve.
Scientists still can't answer what exactly causes the disease. In other words, which factors have the greatest impact on its development. Some researchers believe that lumbosacral osteochondrosis is the price a person pays for walking upright. In fact, the disease has not been observed in animals.
The factors that cause this disease can be divided into external and internal factors. Here are the main reasons that cause it:
- severe spinal injury;
- hereditary;
- flatfoot;
- standing for long periods of time;
- Postural disturbance;
- a sedentary lifestyle;
- being overweight;
- Unbalanced diet.
who is at risk
No one is immune to this disease. Genetic factors determine its more or less predisposition. However, external factors and a person's lifestyle greatly influence the likelihood of developing the disease.
Another cause of this disease is excessive exercise and injury.
Proper nutrition is important for preventing osteochondrosis: food should contain all the necessary components, rich in vitamins and trace elements.
treat
Treatment can be surgical or conservative. If the disease is in the stage of herniation, surgical intervention is essential. Conservative treatment includes the following approaches:
- medical treatement;
- physical therapy and spinal traction;
- massage and manual therapy;
- Physical therapy exercises.
Medications include anti-inflammatory drugs, pain relievers, muscle spasm relievers, and injection blockers. Also used are chondroprotective agents, which reduce pain and promote regeneration of damaged cartilage formation. In some cases, hormonal medications are used.
prevention
Basic principles of preventing lumbosacral osteochondrosis:
- Prevent excessive load on the lower back;
- strengthen back muscles;
- maintain correct posture;
- physical activity;
- proper nutrition;
- Regulation of rest regimes;
- Prompt treatment of other diseases of the back.
home care
practise
There are some very simple exercises that a person can do independently at home. They are used for therapeutic and preventive purposes. Their main task is to strengthen the back muscles to relieve some of the load on the spine.
exercise therapy
Therapeutic exercise is one of the main methods of treating osteochondrosis. Exercise helps strengthen muscles and relieve the burden on the spine. Improves blood circulation in tissues, including intervertebral discs. Therapeutic exercise can help relieve muscle tension and reduce pain.
massage
Massage is an excellent treatment for lumbar osteochondrosis. It improves blood supply to tissues, reduces pain, relieves clips, and strengthens muscle corsets.
rather than the epilogue
To sum up, it can be seen that this disease is the "disease of the century" that truly threatens any modern person.
Osteochondrosis of the lumbosacral spine causes unbearable pain and can become disabled. The disease is difficult to treat, especially in advanced stages.
The positive point is that each of us has the ability to avoid the development of osteochondrosis. All you need to do is take care of your spine: don't put too much pressure on it, watch your weight, maintain a healthy lifestyle, eat normally, and avoid injuries.
Talk to your doctor if you've already started noticing the first symptoms of osteochondrosis. In the initial stages, the disease is easy to treat. Take care of your spine so that even in old age, exercise will bring you joy, not discomfort.

























